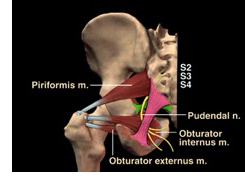
Pudendal neuralgia is a painful condition caused by inflammation or irritation of the pudendal nerve. The pudendal nerve is a somatic nerve within the pelvis comprised of branches of the sacral plexus levels S2-4. The pudendal nerve innervates the external genitalia in men and women including the labia, scrotum, penis, clitoris, and anus and provides motor function for bowel, bladder, and orgasm function. The pudendal nerve has three branches: perineal nerve, inferior rectal, and dorsal penile/clitoral. The pudendal nerve transverses through many other pelvic structures. It passes between the sacrotuberous and sacrospinous ligaments, between the piriformis and coccygeus muscles, adjacent to the ischial spine, and accompanies the pudendal artery and vein through the obturator fascia or Alcock’s (pudendal) canal. Damage or trauma to the pudendal nerve can result from falls onto the coccyx or ischial tuberosities (‘sits” bones), childbirth, abdominal or pelvic surgery, bicycling, horseback riding, sports injuries, squatting or lifting injuries, motor vehicle accidents, faulty biomechanics of the sacroiliac, sacrococcygeal, and hip joints; adverse tension of the pelvic ligaments (sacrotuberous, sacrospinous), pelvic floor muscle dysfunction, pelvic radiation therapy, chronic constipation with habitual straining, and chronic pudendal nerve entrapment. Common symptoms of pudendal neuralgia include pain or impaired sensation in the vulva, vagina, clitoris, penis, scrotum, testicles, rectum, or ischial tuberosities, pain upon sitting, sexual pain/dysfunction such as arousal, erectile, ejaculation, or orgasm; difficulty with urination or bowel movements, constipation, urinary or fecal incontinence, and the sensation of having a foreign object or “fullness” in the vagina, rectum or perineum. Symptoms usually worsen by the end of the day and improve upon lying down or sitting on a toilet seat. Common conditions that could mimic pudendal neuralgia include coccygodynia, sacroiliac joint dysfunction, piriformis syndrome, ischial bursitis, interstitial cystitis, chronic or non-bacterial prostatitis, prostatodynia, vulvodynia, vulvar vestibulitis, chronic pelvic pain syndrome (CPPS), pelvic floor muscle dysfunction (hypertonicity), and proctalgia fugax. Medical testing for proper diagnosis may include an image guided pudendal nerve block, pudendal nerve motor latency test (PNMLT), electromyography (EMG), and an MRI, MRN, or CT scan.
How can Pamela Morrison Physical Therapy, P.C. help Pudendal Neuralgia?
Physical therapy is a proven effective treatment approach for pudendal neuralgia. Your expert pelvic therapist completes a comprehensive history and physical exam. Your physical exam would include evaluation of the spine, pelvic (sacroiliac, sacrococcygeal, pubic symphysis) and hip joints; lower extremity and pelvic soft tissue, muscle, and nerve function; pelvic floor muscle function, adverse neural tissue tension/mobility testing, and visceral mobility testing. Evaluation may also include surface EMG biofeedback of the lower abdominals and pelvic floor muscles. Your evaluation occurs over an hour and half time span to allow adequate time for thoroughness. Once a proper diagnosis and your evaluation findings are established, a prescriptive treatment program will be implemented to meet your individual needs. Treatment may consist of joint mobilization and manipulation to restore proper alignment and joint mobility, soft tissue mobilization (massage, deep tissue, and myofascial release), cross friction massage to pelvic ligaments, scar tissue release/mobilization, specific nerve mobilization/gliding techniques, connective tissue and skin rolling techniques, pain relieving modalities such as TENS, ultrasound, interferential electrical stimulation, cryotherapy, cold laser; stretching exercises, neuromuscular re-education of core muscles and lower extremities, visceral mobilization, and prescriptive strengthening exercises. Pelvic floor muscle rehabilitation occurs including manual therapies and surface EMG biofeedback to focus on down-training or relaxing the pelvic floor muscles. Restoring normal pelvic floor muscle length and resting tone, and releasing painful tender/ trigger points are main treatment objectives. Relieving pain, restoring pudendal nerve mobility and function, and restoring normal bowel, bladder, and sexual function will be primary goals of therapy. This will be achieved through advanced specific manual therapies mentioned above, therapeutic modalities, bowel and bladder re-training as needed, education of proper postural habits and body mechanics, sexual education, and behavioral modification training. Because we are pelvic experts at Pamela Morrison Physical Therapy, we have had tremendous success identifying and treating hundreds of patients with pudendal neuralgia.


