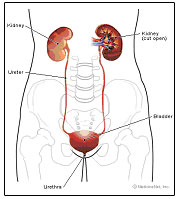
There are different types of incontinence. Urinary incontinence is the inability to control the flow of urine and results in involuntary urination. Stress incontinence is when you leak urine during activities that increase pressure on the bladder such as sneezing, coughing, laughing, jumping, jogging, or lifting. There may be insufficient strength in the muscles supporting the bladder, urethra, and pelvis. The muscles that help support the bladder and resist urination include the pelvic floor muscles and the transversus abdominus, as an accessory. Urge incontinence is when you feel a terrible urge or pressure to urinate and leak on your way to the bathroom and you may leak urine before you reach the bathroom. Some also may experience urge and leak when they put their keys in the front door, when hearing water running, or when outside in the cold weather. Mixed incontinence is when someone has both stress and urge incontinence combined. Fecal incontinence is when you are unable to hold or control stool in the rectum and leak feces. Incontinence can also result from childbirth trauma, pelvic surgeries, consumption of bladder or intestinal irritants, food allergies or sensitivities, prostate issues, hormonal imbalances or deficiencies, a sedentary lifestyle, and neurological diagnoses such as multiple sclerosis, cerebral vascular accident, or spinal cord injury.
How can Pamela Morrison Physical Therapy help with incontinence?
Physical therapy can help all types of incontinence. After a comprehensive physical therapy evaluation with our pelvic expert, it may be determined that weak or incoordinated pelvic floor muscles or trunk (core) muscles are contributing to the problem. Other musculoskeletal issues such as pelvic floor muscle and abdominal trigger points, myofascial tightness, malalignment of pelvic, sacroiliac, spine, and/or hip joints may be a causative or perpetuating factor. Pelvic floor muscle hypertonicity (spasm, pain, shortened, high-tone) can be a causative factor in urge incontinence whereas pelvic floor muscle hypotonicity (weakness, low-tone) can be a causative factor in stress incontinence. Pelvic organ prolapse can also cause incontinence. Thus, your comprehensive evaluation includes close inspection of pelvic floor and core muscle function and tone. Studies have shown that pelvic floor muscle strengthening exercises help with urinary/fecal incontinence. Using our state-of-the art Rehabilitative Real-time ultrasound and surface EMG biofeedback enables the patient to understand the function of pelvic, core and low back muscles in bladder health. Anther modality that may be helpful is neuromuscular electrical stimulation (NMES) to help increase pelvic floor muscle recruitment and hypertrophy or strengthen the muscles. Transvaginal or transrectal NMES is useful in inhibiting the sensation of urge and helps strengthen the pelvic floor muscles rapidly. Trancutaneous electrical nerve stimulation (TENS) has been studied and its use for urinary incontinence proves effective when used over the bladder/suprapubic region and on sacral or tibial nerves. Diet and behavior can also affect incontinence. Food diaries and bladder/bowel voiding diaries are reviewed and changes are implemented to best improve your bladder or rectal function. Behavioral modification techniques are instructed. Core re-training exercises, lower quarter stretching, and pelvic floor muscle overflow exercises are also instructed. Your expert physical therapist at Pamela Morrison Physical Therapy would implement an individualized treatment program to address any issues found during the evaluation.


